
Every year thousands of people in Oakland California arrive at the ED in the acute stages of opioid withdrawal.1 Opioid withdrawal, an agonizing process that involves vomiting, diarrhea, shivering and pain, has historically been treated with an anti-nausea table, a discharge order, and sometimes a list of phone numbers for local drug rehabs. Although not unsympathetic to the plight of the withdrawing opioid user, for a long time, ED physicians lacked better options.
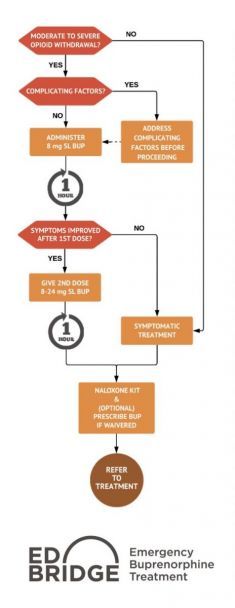
A study, published in 2015 out of Yale-New Haven Hospital, found that patients who were given buprenorphine in the emergency room where twice as likely to be in treatment a month later than those who received the standard of care.2 This study prompted ED physicians to implement medication assisted treatment (MAT) at their home institutions; Dr. Andrew Herring of Highland hospital was one of the first. MAT for opioid addiction usually consists of some combination of buprenorphine, naloxone, and methadone. The goal of MAT is to ease withdrawal symptoms, temper cravings and begin the process of recovery for interested patients.
After securing a small grant from the California Health Care Foundation for Highland and seven other northern California hospitals, Herring began experimenting with administering buprenorphine in the emergency room.1 The logic behind providing MAT in the ED is simple: many opioid users may not interact with medical care systems except in a moment of crises; making sure that MAT is available in the ED is a way to make sure the opportunity is not lost. As Dr. Herring puts it, “People coming in with opioid addiction often want a change and are willing to participate in their treatment. They just don’t know how to get help. There can be this moment in the emergency room, when the patient is in withdrawal and in pain, when we can connect.”3
Outside of these unique ED-based MAT programs, it can be difficult to find a doctor who prescribes buprenorphine. A 2011 study showed that 43% of counties in the United States lacked a single physician who was waivered to prescribe buprenorphine.4 Wait times in some areas can be as long as a year.5 Long wait times for MAT increase the risk of relapse, disease mortality and fatal overdose.6
Although he started with a modest grant, Dr. Andrew Herring’s program (now known as the ED Bridge program), has the state spending $ 700,000 to help expand the program to EDs statewide. This is all part of the greater “California Hub and Spoke system” project which received a $78 million grant for the effort to provide more access to MAT statewide. In addition to his MAT, Herring has been working in his home ED to implement an alternative to opioid pain treatments which utilize regional anesthesia, acupuncture, and meds like lidocaine, gabapentin, ketamine, and magnesium.3
References
- Goodnough, A. (2018, August 18). This E.R. Treats Opioid Addiction on Demand. That’s Very Rare. The New York Times. Retrieved from https://www.nytimes.com/2018/08/18/health/opioid-addiction-treatment.html
- D’Onofrio, G., O’Connor, P. G., Pantalon, M. V., Chawarski, M. C., Busch, S. H., Owens, P. H., … Fiellin, D. A. (2015). Emergency Department–Initiated Buprenorphine/Naloxone Treatment for Opioid Dependence: A Randomized Clinical Trial. JAMA, 313(16), 1636–1644. https://doi.org/10.1001/jama.2015.3474
- Firth, Andrea A. (2017, October 16). Facing the Opioid Emergency. Retrieved January 29, 2019, from http://www.oaklandmagazine.com/October-2017/Facing-the-Opioid-Emergency/
- Stein, B. D., Pacula, R. L., Gordon, A. J., Burns, R. M., Leslie, D. L., Sorbero, M. J., … Dick, A. W. (2015). Where Is Buprenorphine Dispensed to Treat Opioid Use Disorders? The Role of Private Offices, Opioid Treatment Programs, and Substance Abuse Treatment Facilities in Urban and Rural Counties. The Milbank Quarterly, 93(3), 561–583. https://doi.org/10.1111/1468-0009.12137
- Vestal, Christine. (2016, February 11). Waiting Lists Grow for Medicine to Fight Opioid Addiction. Retrieved January 29, 2019, from http://pew.org/1Q9w1mc
- Sigmon, S. C., Meyer, A., Hruska, B., Ochalek, T., Rose, G., Badger, G. J., … Schwartz, R. P. (2015). Bridging waitlist delays with Interim Buprenorphine Treatment: Initial feasibility. Addictive Behaviors, 51, 136–142. https://doi.org/10.1016/j.addbeh.2015.07.030
Rebecca Siegel, is a research fellow in the GWU Department of Emergency Medicine and a medical student at Ben Gurion University in Israel.